Health Inequalities arise when barriers hinder individuals and communities from accessing optimal conditions for reaching their full potential. It distinguishes inequities from health disparities, which are differences in health status linked to social or demographic factors. Health Equity involves valuing everyone equally, optimizing conditions across various life stages, and collaborating with different sectors to address factors influencing health, such as employment, housing, education, healthcare, public safety, and food access. Notably, the passage acknowledges racism as a factor influencing the distribution of these social determinants.
According to the Centers for Disease Control and Prevention (CDC), addressing disparities necessitates national leadership to involve diverse stakeholders, coordinate federal entities and nonfederal partners, advocate for effective policies, and ensure accountability. The CDC and its collaborators can utilize the report’s findings to heighten awareness of vulnerable groups. Additionally, the insights can motivate increased interventions at state, tribal, and local levels to tackle health disparities and inequalities effectively.
Also, Healthy People 2030 offers diverse strategies for attaining health equity. A pivotal aspect in realizing the overarching vision of enhancing the health and well-being of all is the targeted addressing of health disparities. Consequently, disparity ratios are being formulated to evaluate data on disparities for population-based core objectives, utilizing demographic group data available at a specific time point.
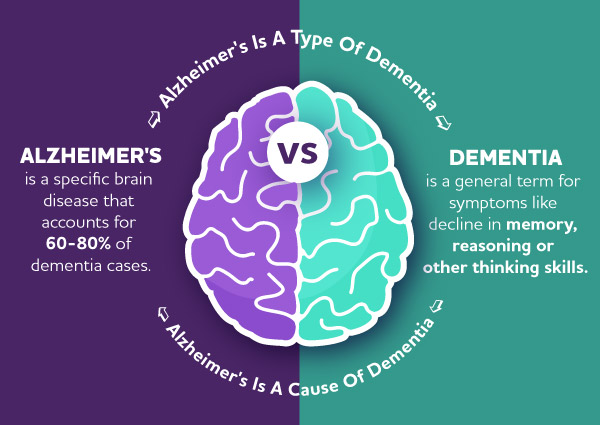
In Alzheimer’s disease, achieving health equity gains significant importance. Factors such as income, education, and access to health care can create disparities in diagnosis, treatment, and support services. We address all disparities so that patients and caregivers have equal opportunities for early detection, quality care, and support services regardless of their background. This approach is crucial for creating an inclusive society where everyone can age with dignity and receive the necessary assistance in managing the challenges posed by Alzheimer’s disease.
https://www.apha.org/Topics-and-Issues/Health-Equity
https://www.cdc.gov/minorityhealth/CHDIReport.html
https://health.gov/healthypeople/objectives-and-data/about-disparities-data
https://www.nimhd.nih.gov/resources/understanding-health-disparities/health-equity.html